An Interview with Dr. George Fernaine
In Nov. 2018 the American College of Cardiology and American Heart Association released new guidelines on managing cholesterol to minimize the risk of heart attack, stroke and death. This is the first time the guidelines have been updated since 2013. They recommend a more detailed, personalized approach in risk assessments and advocate for more aggressive treatment with statin therapy and getting low-density lipoprotein cholesterol (LDL-C, or commonly referred to as “bad cholesterol”) to target level — generally less than 100 mg/dL; and, for those with risk factors, less than 70 mg/dL. As stated in the guideline’s preamble, “Guidelines are intended to define practices meeting the needs of patients in most, but not all, circumstances, and should not replace clinical judgment.” This document is available on the websites of the American College of Cardiology (www.acc.org) and the American Heart Association (professional.heart.org).

Dr. George Fernaine, chief of cardiology at NYU Langone Hospital — Brooklyn, spoke with us and discussed what LDL-C levels people should strive for; the use of statins; and how people can control their cholesterol levels with lifestyle modifications.
RHSR: In layman’s terms, what are the biggest changes to the guidelines, and what can people do to better adhere to them?
GF: I think the big take-home message is that you really have to reduce your cholesterol in order to reduce the risk of atherosclerotic cardiovascular disease, the potential of having strokes, heart attacks and aneurysms. So what you can do is eat a healthier, prudent diet — try to stay away from salt, fast food, fatty meats; concentrate more on fish, chicken [and] turkey. Increase your exercise activity to five times a week and cardiovascular exercise more so than just lifting. It’s important to see a doctor, even as early as the age of 20 to see whether you’re at risk for heart disease and to have your cholesterol checked. Cholesterol issues start happening at an early age, even before you’re a teenager, so one of the best things parents can do is to teach kids how to eat properly at a young age so they don’t develop bad habits.
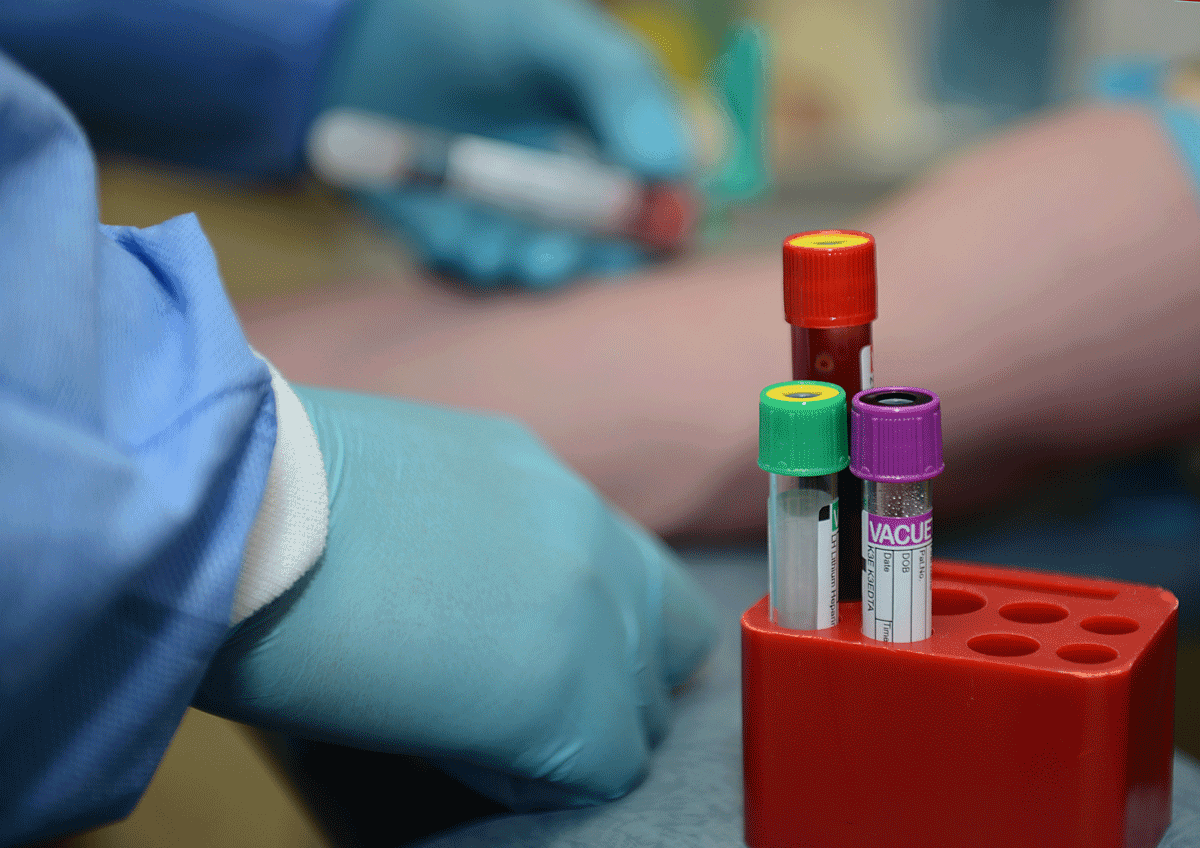
RHSR: How often should people check their cholesterol levels?
GF: It depends on your risk profile. You should check it once [a year]. If it’s normal and your risk profile isn’t too bad, [check it] every 12 months or a little over every 12 months. If it’s high and something that requires medication or dietary modification, you may have to check it every three months until you get it under control.
RHSR: What LDL-C levels should people strive for?
GF: Again, it all depends on your risk profile. For example, sometimes the goal is just to reduce it by 50% of what you started off with, depending on your risk profile. If you’ve had a heart attack or a stroke, the hard number is 70 or less. It’s definitely a moving target. People don’t understand that they can see their doctor and their cholesterol is fine — and that’s absolutely true. But within that year, if you develop diabetes or you’ve had a heart attack, all of a sudden what would’ve been a normal cholesterol for you, without those conditions, becomes extremely abnormal.
RHSR: Can you explain the use of statins?
GF: They’re cholesterol medications that reduce LDLs, which is what you consider the “bad cholesterol.” It’s shown to decrease the incidence of heart attacks and strokes, the progression of atherosclerotic disease [and] buildup of plaque. The [most common] risks that you have to pay attention to are a rise in liver function tests, muscle pains and joint pains. If you develop that with a statin, then you should see a doctor who will do blood tests and maybe either switch around the medications or provide you with alternate medications.
Author
-

George Fiala has worked in radio, newspapers and direct marketing his whole life, except for when he was a vendor at Shea Stadium, pizza and cheesesteak maker in Lancaster, PA, and an occasional comic book dealer. He studied English and drinking in college, international relations at the New School, and in his spare time plays drums and fixes pinball machines.
View all posts
George Fiala has worked in radio, newspapers and direct marketing his whole life, except for when he was a vendor at Shea Stadium, pizza and cheesesteak maker in Lancaster, PA, and an occasional comic book dealer. He studied English and drinking in college, international relations at the New School, and in his spare time plays drums and fixes pinball machines.